Periodontitis: A Comprehensive Overview
Introduction
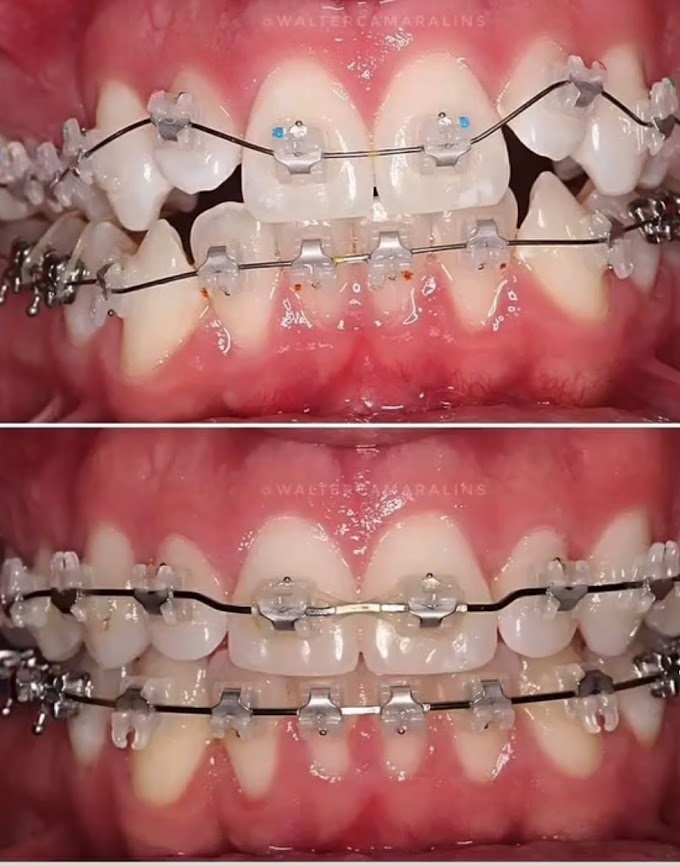
Periodontitis is a chronic biofilm-induced inflammatory condition that significantly affects overall health. It primarily involves the tooth-supporting tissues, including the gingiva, periodontal ligament, and alveolar bone 1. Dental plaque accumulation at the gingival margin initiates an inflammatory response, leading to microbial alterations and potentially drastic consequences in susceptible individuals.
Understanding Periodontitis
Gingivitis vs. Periodontitis:
- Gingivitis refers to inflammation of the gingiva (gums) and is the earliest stage of gum disease. It often results from inadequate oral hygiene, causing dental plaque buildup along the gumline. Common signs include swollen, tender gums, bleeding during brushing or flossing, and bad breath.
- Periodontitis, on the other hand, is a more advanced stage. It occurs when gingivitis progresses, leading to irreversible damage. In periodontitis, the tissues around the teeth (including bone) become affected, resulting in pocket formation, gum recession, and potential tooth mobility.
Mechanical Debridement (Scaling and Root Planing):
- The standard treatment for periodontitis involves mechanical plaque control, known as scaling and root planing. However, this approach may not fully remove subgingival plaque and calculus, especially in deep pockets and furcation defects 2.
- Despite its limitations, scaling and root planing remain essential for managing periodontitis.
Adjunctive Therapy with Locally Delivered Antibiotics:
- To enhance treatment outcomes, researchers have explored the use of locally delivered antibiotics alongside mechanical debridement.
- Studies consistently show improvements when antibiotics are added to the treatment regimen. These improvements include reduced probing depths, gingival inflammation, and bleeding on probing.
- Additionally, clinical attachment level and periodontal pocket depth reduction are observed with adjunctive antibiotic therapy.
Choosing the Right Antibiotic:
- While individual antimicrobial agents have shown effectiveness, determining the best local antibiotic remains challenging. Each product has unique features, making direct comparisons difficult.
- Local administration of antibiotics into the periodontal pocket can be a valuable adjunct to mechanical instruments.
Signs and Diagnosis
- Common signs of periodontitis include:
- Bad breath
- Tender or sensitive gums
- Bleeding during brushing or flossing
- Gum recession
- Loose or shifting teeth
- Soreness when biting down
- Changes in occlusion (how teeth bite together)
- Notably, smokers may not always exhibit bleeding, swelling, or redness despite having gum disease. Regular gum exams are crucial for tobacco users.
In summary, periodontitis is a multifaceted disease that demands comprehensive management. Combining mechanical debridement with locally delivered antibiotics can significantly improve clinical outcomes. If you suspect periodontitis, seek professional evaluation promptly to prevent irreversible damage 34.
Remember to maintain good oral hygiene practices, and regular dental visits are essential.
for more dental articles kindly visit:
https://www.fixedbracesblog.com/
detection and effective management. Feel free to reach out if you have any further questions or need additional information! 😊🦷🌟